Перейти в eShop
Перейти в eShop

SLActive - УНІКАЛЬНА АКТИВНА ПОВЕРХНЯ
Унікальна запатентована активна поверхня з чіткими наноструктурами, які збільшують площу контакту з кісткою на 50%

ВДВІЧІ ШВИДШЕ ЗАГОЮВАННЯ
Наноструктури поверхні SLActive забезпечують мінералізацію кісткових клітин та вдвічі пришвидшують процеси остеоінтеграції

ПЕРЕДБАЧУВАНИЙ РЕЗУЛЬТАТ
100% приживленість, навіть у пацієнтів групи ризику - діабет 2 типу, курці, пацієнти, які мали променеву та хіміотерапію

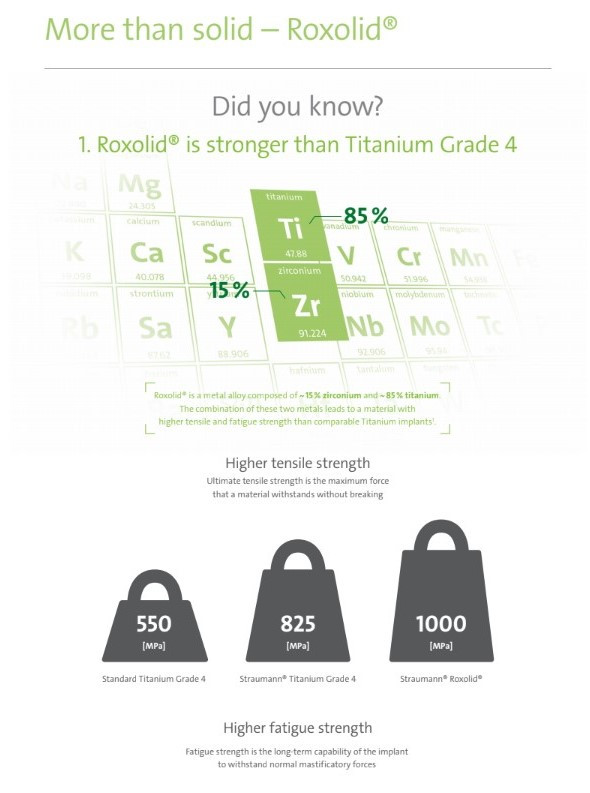
ROXOLID - УНІКАЛЬНА ЗАПАТЕНТОВАНА РОЗРОБКА
Унікальна запатентована розробка Straumann, сплав титану (85%) та цирконію (15%)

НАДМІЦНИЙ СПЛАВ ІМПЛАНТАТУ
Roxolid на 35% міцніший за титан, що дозволяє використання імплантатів меншого діаметру та довжини порівняно з титановими імплантатами

БІОЛОГІЧНО-СУМІСНИЙ СПЛАВ
На 1,6% вищий показник приживлення в порівнянні з титаном завдяки вмісту у сплаві біологічно сумісного цирконію
Читати
Відео
ImpulsePlay

Підписатись на новини
Натискаючи кнопку, ви автоматично
погоджуєтесь на обробку персональних даних
СПИСОК ЛІТЕРАТУРИ
- Nicolau P, Guerra F, Reis R, Krafft T, Benz K , Jackowski J 10-year results from a randomized controlled multicenter study with immediately and early loaded SLActive implants in posterior jaws. Accepted for oral presentation at 25th Annual Scientific Meeting of the European Association of Osseointegration – 29 Sep – 1 Oct 2016, Paris.
- Patients treated with dental implants after surgery and radio-chemotherapy of oral cancer. Heberer S, Kilic S, Hossamo J, Raguse J-D, Nelson K. Rehabilitation of irradiated patients with modified and conventional sandblasted, acid-etched implants: preliminary results of a split-mouth study. Clin. Oral Impl. Res. 22, 2011; 546–551.
- Straumann SLActive implants compared to Straumann SLA implants. Lang NP, Salvi GE, Huynh-Ba G, Ivanovski S, Donos N, Bosshardt DD. Early osseointegration to hydrophilic and hydrophobic implant surfaces in humans. Clin Oral Implants Res. 2011 Apr;22(4):349-56. doi: 10.1111/j.1600-0501.2011.02172.x;Rupp F, Scheideler L, Olshanska N, de Wild M,Wieland M, Geis-Gerstorfer J. Enhancing surface free energy and hydrophilicity through chemical modification of microstructured titanium implant surfaces. Journal of BiomedicalMaterials Research A, 76(2):323-334, 2006. ; De Wild M. Superhydrophilic SLActive® implants. Straumann document 151.52, 2005 ; Katharina Maniura. Laboratory for Materials – Biology Interactions Empa, St. Gallen, Switzerland Protein and blood adsorption on Ti and TiZr implants as a model for osseointegration. EAO 22nd Annual Scientific Meeting, October 17 – 19 2013, Dublin ; Schwarz, F., et al., Bone regeneration in dehiscence-type defects at non-submerged and submerged chemically modified (SLActive®) and conventional SLA® titanium implants: an immunohistochemical study in dogs. J Clin.Periodontol. 35.1 (2008): 64–75. ; Rausch-fan X, Qu Z, Wieland M, Matejka M, Schedle A. Differentiation and cytokine synthesis of human alveolar osteoblasts compared to osteoblast-like cells (MG63) in response to titanium surfaces. Dental Materials 2008 Jan;24(1):102-10. Epub 2007 Apr 27. ; Schwarz F, Herten M, Sager M, Wieland M, Dard M, Becker J. Histological and immunohistochemical analysis of initial and early osseous integration at chemically modified andconventional SLA® titanium implants: Preliminary results of a pilot study in dogs. Clinical Oral Implants Research, 11(4): 481-488, 2007. Raghavendra S, Wood MC, Taylor TD. Int. J. Oral Maxillofac. Implants. 2005 May–Jun;20(3):425–31. Oates TW, Valderrama P, Bischof M, Nedir R, Jones A, Simpson J, Toutenburg H, Cochran DL. Enhanced implant stability with a chemically modified SLA® surface: a randomized pilot study. Int. J. Oral Maxillofac. Implants. 2007;22(5):755–760
- Yerit, K., Posch, M., Seemann, M., Hainich, S., Dortbudak, O., Turhani, D., Ozyuvaci, H., Watzinger, R. and Ewers, R. (2006) Implant Survival in Mandibles of Irradiated Oral Cancer Patients. Clinical Oral Implants Research, 17, 337-344. http://dx.doi.org/10.1111/j.1600- 0501.2005.01160.x.
- Verdonck, H.W.D., Meijer, G.J., Laurin, T., Nieman, F.H.M., Stoll, C., Riediger, D., Stoelinga, P.J.W. and de Baat, C. (2007) Assessment of Vascularity in Irradiated and Non-Irradiated Maxillary and Mandibular Alveolar Minipig Bone Using Laser Doppler Flowmetry. International Journal of Oral Maxillofacial Implants, 22, 774-778.
- Hu, W.W., Ward, B.B., Wang, Z. and Krebsbach, P.H. (2010) Bone Regeneration in Defects Compromised by Radiotherapy. Journal of Dental Research, 89, 77-81. http://dx.doi.org/10.1177/0022034509352151.
- Wang, R., Pillai, K. and Jones, P.K. (1998) Dosimetric Measurements of Scatter Radiation from Dental Implants in Stimulated Head and Neck Radiotherapy. International Journal of Oral Maxillofacial Implants, 13, 197-203.
- Grotz, K.A., Al-Nawas, B., Piepkorn, B., Reichert, T.E., Duschner, H. and Wagner, W.(1999) Micromorphological Findings in Jaw Bone after Radiotherapy. Mund-, Kiefer- und Gesichtschirurgie, 3, 140-145.
- Chambrone L, Mandia J, Shibli JA, Romito GA, Abrahao M. Dental Implants Installed in Irradiated Jaws: A Systematic Review. Journal of Dental Research. 2013;92(12 Suppl):119S-130S. doi:10.1177/0022034513504947.
- Shugaa-Addin B, Al-Shamiri H-M, Al-Maweri S, Tarakji B. The effect of radiotherapy on survival of dental implants in head and neck cancer patients. Journal of Clinical and Experimental Dentistry.2016;8(2):e194-e200. doi:10.4317/jced.52346.
- Nooh N. Dental implant survival in irradiated oral cancer patients: a systematic review of the literature. Int J Oral Maxillofac Implants. 2013 Sep-Oct;28(5):1233-42. doi: 10.11607/jomi.3045.
- Dholam KP, Gurav SV. Dental implants in irradiated jaws: A literature review. J Can Res Ther [serial online] 2012 [cited 2016 Aug 17];8:85-93. Available from: http://www.cancerjournal.net/text.asp?2012/8/6/85/92220.
- Nelson, K., Stricker, A., Raguse, J.-D. and Nahles, S. (2016), Rehabilitatio of irradiated patients with chemically modified and conventional SLA implants: a clinical clarification. J Oral Rehabil, 43: 871–872. doi:10.1111/joor.12434
- C. NACK, J.-D. RAGUSE, A. STRICKER , K. NELSON & S. NAHLES. Rehabilitation of irradiated patients with chemically modified and conventional SLA implants: five-year follow-up. Journal of Oral Rehabilitation 2015 42; 57—64.
- Devlin H, Garland H, Sloan P. Healing of tooth extraction sockets in experimental diabetes mellitus. J. of Oral Maxillofac. Surg. 1996; 54:1087-1091
- Wang F1, Song YL, Li DH, Li CX, Wang Y, Zhang N, Wang BG. Type 2 diabetes mellitus impairs bone healing of dental implants in GK rats. Diabetes Res Clin Pract. 2010; 88:e7-9.
- IDF Diabetes Atlas, 7th Edition, 2015 http://www.diabetesatlas.org/.
- US Centers for Disease Control and Prevention. Diabetes 2014 report card. Available from: www.cdc.gov/diabetes/library/reports/congress.html. Accessed September 2015.
- Machuca G., Cabrera J.J. “A prospective, case-control clinical study of titanium-zirconium allow implants with hydrophilic surface in patients with Type 2 diabetes mellitus” Manuscript accepted.
- Hotchkiss KM, Ayad NB, Hyzy SL, Boyan BD, Olivares-Navarrete R. Dental implant surface chemistry and energy alter macrophage activation in vitro. Clin. Oral Impl. Res. 00, 2016, 1–10. doi: 10.1111/clr.12814.
- Lee R, Hamlet SM, Ivanovski S. The influence of titanium surface characteristics on macrophage phenotype polarization during osseous healing in type I diabetic rats: A pilot study. Clin Oral Impl Res (accepted 4/8/2016).
- Straumann (2016). SLActive supports enhanced bone formation in a minipig surgical GBR model with coronal circumferential defects. Unpublished data.
- Müller E, Rottmar M, Guimond S, Tobler U, Stephan M, Berner S, Maniura K The interplay of surface chemistry and (nano-)topography defines the osseointegrative potential of Roxolid® dental implant surfaces. eCM Meeting Abstracts 2017, Collection 3; SSB+RM (page 31).
- EMPA (2017) Report additional experiments: Impact of RXD SLA, RXD SLAnano, RXD SLActive, and RXD pmod SLA surfaces on protein adsorption, blood coagulation, and osteogenic differentiation of HBCs. Final report: Impact of RXD SLA, RXD SLAnano, RXD SLActive, and RXD pmod SLA surfaces on protein adsorption, blood coagulation, and osteogenic differentiation of HBCs. EMPA, Swiss Federal Laboratories for Materials Science and Technology (data on file).
- Strauamnn (2017) Developed area ratio by nanostructures on Rxd modMA surface. Report SR0748. Unpublished data.
- Wennerberg A, Albrektsson T. On implant surfaces: a review of current knowledge and opinions. Int J Oral maxillofac Implants 2009: 24:63-74
- Kopf BS, Ruch S, Berner S, Spencer ND, Maniura-Weber K. 2015. The role of nanostructures and hydrophilicity in osseointegration: In-vitro protein-adsorption and blood-interaction studies. J Biomed Mater Res Part A2015:103A:2661–2672.
- xWennerberg A, Jimbo R, St€ubinger S, Obrecht M, Dard M, Berner S. Nanostructures and hydrophilicity influence osseointegration – A biomechanical study in the rabbit tibia. Clin. Oral Impl. Res. 25, 2014, 1041–1050doi: 10.1111/clr.12213
- Chrcanovic BR, Albrektsson T, Wennerberg A Smoking and dental implants: A systematic review and meta-analysis. J Dent. 2015 May;43(5):487-98
- ChenY, Man Y Clinical evaluation of SLActive Titaniumzirconium narrow diameter implants for anterior and posterior crowns in smokers and nonsmokers group. Presented at the ITI World Symposium, Basel, May4-6, 2017 Abstract booklet: Clinical Research 045, p18.
- Hotchkiss K.M, Sowers K.T, Olivares-Navarrete R. Clinical Implants Differentially Modulate Inflammatory Response and Osteogenic Differentiation. Presented at 95th General Session of International Association for Dental Research, USA, March 22-25, 2017. https://iadr2017.zerista.com/event/member?item_id=5725415
- Hsu JT, Shen YW, Kuo CW, Wang RT, Fuh LJ, Huang HL. Impacts of 3D bone-to- implant contact and implant diameter on primary stability of dental implant. J Formos Med Assoc. 2017 Aug;116(8):582-590. ;
- Buser D, Schenk RK, Steinemann S, Fiorellini JP, Fox CH, Stich H. Influence of surface characteristics on bone integration of titanium implants. A histomorphometric study in miniature pigs. J Biomed Mater Res. 1991 Jul;25(7):889-902 ;
- Smeets R, Stadlinger B, Schwarz F, Beck-Broichsitter B, Jung O, Precht C, Kloss F, Gröbe A, Heiland M, Ebker T. Impact of Dental Implant Surface Modifications on Osseointegration. Biomed Res Int. 2016;2016:6285620. ;
- Goyal N., Priyanka R. K. Effect of various implant surface treatments on osseointegration – a literature review. Indian Journal of Dental Sciences. 2012;4:154–157 31
- Cabrera-Domínguez J. A prospective, two-year clinical trial of titanium-zirconium alloy implants (Roxolid® Straumann®) with hydrophilic surface (SLActive®) in patients with Type 2 Diabetes Mellitus. presented during 26th Annual Scientific Meeting of the European Association of Osseointegration – 5-7 Oct 2017, Madrid, Spain.
 Назад
Назад